Recurrent Lower Urinary Tract Infection (UTI)
What is a Urinary Tract Infection?
Urinary tract infections (UTIs) are common and can be painful and uncomfortable,but they can be easily treated with a course of antibiotics.
UTIs aremore common in women than in men. Up to half the population of women will suffer a urinary tract infection (UTI) within their lifetime, of which 25−35% will have a recurrent UTI within 3−6 months.
A recurrent UTI is defined as three or more uncomplicated infections documented by urine culture in the last 12 months.
Symptoms of Lower UTI
- Pain or a burning sensation when urinating (doctors refer to this as dysuria)
- Frequency: a need to urinate often during the day and the night
- A constant, dull pain in the suprapubic region, and a bad smell of urine.
- Cloudy urine or blood in your urine (haematuria)
- Back pain
- A general sense of feeling unwell
Causes of urinary tract infections
Most UTIs are caused by bacteria that live in the digestive system. The bacteria can spread to the urethra via the anus. For example, if toilet paper touches your anus and then touches your genitals, the bacteria can multiply and move through your urinary tract.
Who’s at risk of getting a UTI?
Women are more likely than men to have a UTI because in women, the urethra is closer to the anus and is much shorter, making it easier for bacteria to reach the bladder.
You are also more likely to develop a UTI if you have:
- A condition that obstructs or blocks your urinary tract, such askidney, ureter and bladder stones.
- High post-void residual volume: a condition that prevents you fully emptying your bladder (it’s easier for bacteria to multiply if urine stays in the bladder for too long)
- A weakened immune system from chemotherapy or HIV for example.
- a urinary catheter– a tubeinsertedinto your bladder to drain away the urine.
- Others: poorly controlled diabetes, cystocele or rectocele, poor fluid intake and constipation
Further risk factors in women
Womenare also more likely to get a UTI if:
- Constipation
- They’re sexually active – having sex can irritate the urethra, allowing bacteria to travel through it more easily and into the bladder
- They use adiaphragmfor contraception, as a diaphragm can put pressure on the bladder and prevent it emptying properly
- They usecondomscoated in spermicide, as spermicide can irritate the vagina, making it more vulnerable to infection
- Lack of estrogen after menopause (atrophic vaginitis).
Diagnosis
- Aurine test which can detect bacteria and blood in the urine (mid-stream urine culture).
- A blood test to assess the kidney function (not mandatory).
- Ultrasound scan of the kidney, ureter, and bladder to assess if there is any urological abnormalities, stones, and high post-void residual volume.
Treatment
First LineTreatment:
- Increase oral fluids, mainly water (>2 liters a day)
- Drinking small amount of cranberry juice (300 mls/day) as it stops the bacteria sticking to the bladder wall.
- Antibiotics according to the urine culture and bacterial sensitivity.
- Local vaginal estrogen cream in post-menopausal patients.
- Cystoscopy and urethral dilatation if there is high post-void residual volume.
- Treatment of other urological abnormalities. For example, treatment of urinary stones, or correction of cystocele or rectocele.
Second Line Treatment:
If the UTI recurred, it can be treated as above plus:
- Prophylactic antibiotics: small dose of antibiotic in the evening for 4 months or after intercourse if the infection is related to intercourse).
The prophylactic antibiotic will be changed every 4-6 months to avoid bacterial resistance.
- Non-Antibiotic prevention: using D-Mannose, Methenamine Hippurate, cranberry etc.
- Intravesical installation of Glycosaminoglycan (GAG) (iAluRil®): If there is still recurrence of UTI the next step would be to use intravesical (inside the bladder) instillation of combination of GAG, (iAluRil®) (Hyaluronic Acid and Chondroitin).
- Recent studies show that by using intravesical GAG there is a reduction in UTIs up to 70% in comparison to placebo and that intravesical treatment is more effective than low dose antibiotic prophylaxis.
What is Glycosaminoglycan (GAG) (iAluRil®)?
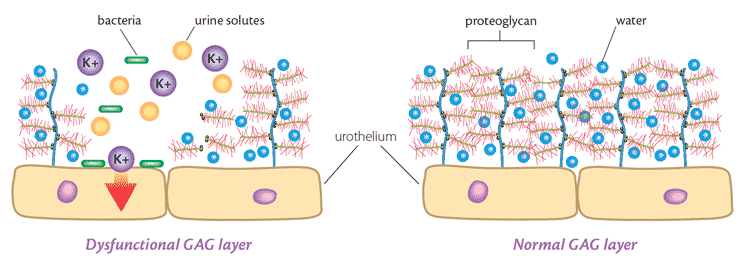
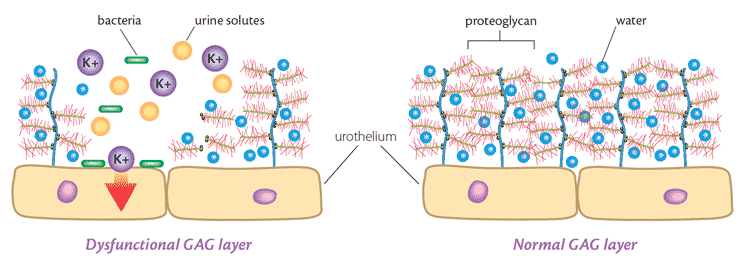
In a healthy bladder there is a natural barrier that protects the bladder lining from the urine. This barrier is called the glycosaminoglycan (GAG) layer. If this barrier is damaged, urine comes into direct contact with the tissues of the bladder lining and over time can cause damage to these tissues. iAluRil contains two of the natural GAGs that form this barrier; hyaluronic acid (HA) and chondroitin sulfate (CS). By administering iAluRil directly into the bladder, these GAGs help to repair the damage to the GAG layer and restore the bladder’s protective coating, preventing recurrent UTI.
How is GAG administered?
GAG is instilled directly into the bladder. The procedure is quite painless and may be undertaken in a hospital/clinic, or self-administered following instruction from a Health Care Professional. For best results, Hyaluronic Acid should be retained in the bladder for as long as possible (a minimum of 30 minutes).
How long do I need treatment for?
GAG is administered initially once weekly for four consecutive weeks, then once monthly for 4 months. You may need a top up course: 3 weekly doses every 3 months.
Potential side effects are minor and include mild bladder pain and small risk of urine infection and blood in the urine.